Overdose deaths from opioids are down over the last year, opioid prescriptions have plummeted by 44% in the last decade, National settlements have been reached with Janssen, Cardinal, McKesson, AmerisourceBergen, Teva, Allergan, CVS, Walgreens, Walmart, and Kroger Co. 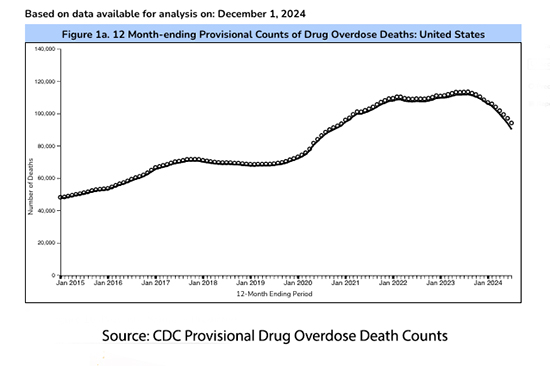 The Purdue settlement suffered a setback in July but appears still a work in progress. In the opioid crisis, it seems “victory,” even if a bit pyrrhic is at hand.
The Purdue settlement suffered a setback in July but appears still a work in progress. In the opioid crisis, it seems “victory,” even if a bit pyrrhic is at hand.
Despite the good news, could a dark cloud be fabricated to obscure the silver lining? What will the experts, who have earned large fees from courtroom testimony, and advocacy groups allocated millions for opioid settlements do when the cash-cow, at least for them, of opioid scares fades away? We need look no further than the “thought leader for the anti-opioid crowd, Dr. Andrew Kolodny." [1]
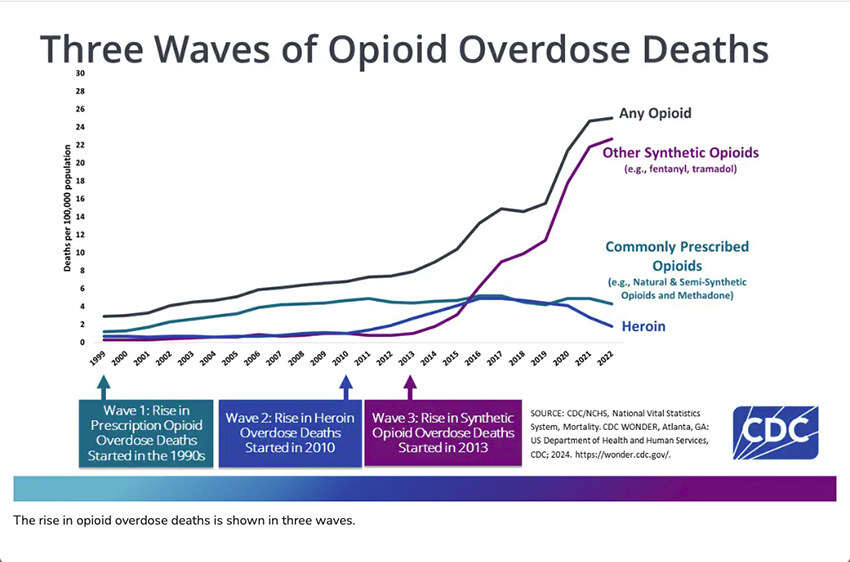
One of the major problems Dr. Kolodny has faced in his personal anti-opioid war is that most of the carnage is related to the non-prescriptive use of illicit opioids. This graphic from the CDC demonstrates clearly that our opioid crisis is not primarily due to prescriptions written by physicians. Nor do the data show that they have ever, been a significant driver. But creating policy to control physicians and influencing CDC guidelines is far easier than dealing with cartels.
Dr. Kolodny, in his effort to both minimize any sense of progress and to reignite the war on prescription opioids has turned to the “National Survey on Drug Use and Health (NSDUH), one of the primary tools used by the federal government for substance-use surveillance, consistently reported low rates of OUD.” He claims that, in the past, the surveyors have made a fundamental error in collecting their information believing that opioid use disorder (OUD) can occur in patients taking prescription drugs only if they misuse their medications. Under that assessment, only 1.6 million people were reported to have OUD.
In 2021, HHS redefined OUD to align with the DSM-5 criteria. As would be expected estimates of individuals in the US with OUD rose, to 6.1 million. Furthermore, taking into account those not reporting symptoms, the number rises still further to 9.4 million. These numbers prompted the good doctor to write,
“The discovery of millions of previously undetected cases of OUD should prompt an urgent investigation to improve understanding of the overlooked population.”
In essence, the rise is because, individuals given prescriptions for opioids who do not misuse the drug, 62% of the estimated rise, are now considered to have OUD because they
“were unsuccessful [in]efforts to cut down or control use, opioid craving, and [in] spending a great deal of time obtaining or using opioids or recovering from opioid use.”
But is OUD the only explanation for those symptoms? Dr. Kolodny does give lip-service to other explanations, especially the time involved in obtaining or using opioids, “because many prescribers have become more reluctant to treat patients with opioids for long periods.” What he fails to mention is that this reluctance is the fruit of his efforts along with others to demonize the appropriate medical use of opioids resulting in a medical landscape where these prescriptions are a red flag. It takes a great deal of chutzpah (a Yiddish term for audacity) to decry the condition you created.
Opioid craving, is “an overwhelmingly strong desire or need to use a drug,” which will go hand in hand with unsuccessful efforts to cut down or control opioid use. But is it truly a craving when opioids are the only medication that provides a quality of life? Is it the patient unsuccessful when in consultation with their physician they increase the dosage or create different medication usages [2] to meet their clinical needs?
Kolodny continues:
“Although some of these patients appear to function well using long-term opioids, the new findings suggest that a large group of patients who are taking opioids as prescribed may nevertheless have OUD. The findings may also help explain why some patients are unable to taper off opioids and why switching to buprenorphine, a first-line treatment for OUD, often improves outcomes. It’s been known for decades that proper management of OUD generally involves long-term opioid maintenance therapy.”
This quote is perhaps Dr. Kolodny at his best, speaking from both sides of his mouth. If a patient is indeed functioning well, then where is the disorder? Certainly, a functional assessment is more valid than a DSM checklist. And if an individual is unable to taper off opioids, one of the hallmarks of OUD, then how is switching to buprenorphine, an opioid with a different, albeit “safer” profile, an improved outcome?
“Evidence that 4.8 million patients who have been prescribed opioids for pain may have OUD should reinforce calls for more cautious use of opioid analgesics, including use for acute pain, which has often been the starting point for long-term use.” [emphasis added]
Since 2011 physicians have reduced prescriptions for opioids by 44%. The refills of an initial prescription vary with the condition, but on average 25% of a 7-day prescription are refilled, that number drops to roughly 6% at one year.
Can Dr. Kolodny say, with clarity that that 6% reflects OUD or could it reflect a chronic pain pattern that has been unresponsive to other therapies? He goes on to point out that that the rate of decrease in postoperative opioid prescriptions has slowed, evidently a sign that “clinicians continue to overprescribe opioids;” or is it that we have found the lower limit on what can be considered humane, efficacious care?
Dr. Kolodny’s redefinition of OUD is a masterclass in manufacturing a crisis where one no longer exists. By conflating effective pain management with addiction, he has created a statistical mirage that serves only to stigmatize chronic pain patients and bolster his anti-opioid crusade. As the data reveals a sharp decline in opioid prescriptions and overdose deaths, his narrative grows increasingly disconnected from reality, leaving chronic pain sufferers to navigate a medical system terrified of treating them. Perhaps it’s time to shift the focus from scoring ideological points to addressing the real opioid crisis: illicit drug use and the systemic failures that allow it to persist. In the end, true progress comes not from inflating statistics, but from addressing facts with compassion and precision.
[1] The article is co-written by Dr. Robert Bohler, who self-describes himself as "as a recovery scientist with an emphasis in opioid use disorder."
[2] Pain management protocols often involve the use of a daily long-acting medication to tamp down the background pain and additional acute or rescue doses of a more fast-acting opioid to treat flare-ups.
Screened Out — How a Survey Change Sheds Light on Iatrogenic Opioid Use Disorder NEJM DOI: 10.1056/NEJMp241091



