
Frederick McKay’s journey west in the early 1900s was fueled by health concerns common at the time—he, like many others thought to be tubercular, sought relief in "a veritable Eden for consumptive invalids," Colorado’s dry climate. Colorado Springs, his destination, was experiencing explosive growth owing to gold strikes in nearby Cripple Creek, and McKay’s skills as a dentist were quickly in demand. From the outset, he noticed something peculiar about local teeth: brown stains, later dubbed “Colorado Brown Stain,” disfigured many residents’ smiles. Early theories blamed poor milk quality, high-calcium water, or specific diets (such as too much pork), but McKay found no conclusive explanation. Despite his curiosity, he set the question aside for nearly a decade, focusing instead on establishing his practice and studying orthodontia back east.
By 1908, the problem persisted, and community leaders, worried about the negative attention the stains brought upon their burgeoning city, prodded the local dental society to act. Funded by just $21, three dentists surveyed nearly 3,000 students and discovered that 87.5% had signs of this staining. Such a high prevalence demanded a deeper investigation.
Enter Dr. G.V. Black
Seeking an expert partner, McKay reached out to Dr. G.V. Black of Northwestern University, a leading figure in American dentistry. Initially skeptical, Dr. Black visited Colorado Springs and immediately saw the gravity of the situation.
"I found it prominent in every group of children. One does not have to search for it, for it is continually forcing itself on the attention of the stranger by its persistent prominence. This is much more than a deformity of childhood. If it were only that, it would be of less consequence, but it is a deformity for life." – Dr. G.V. Black
Dr. Black’s public endorsement of McKay’s observation proved a tipping point. He presented his findings in a talk titled “Developmental Faults in Enamel and the Resulting Brown Stain” and emphasized the strange corollary that while the stains were unsightly, affected teeth were unusually resistant to decay. However, neither he nor McKay could pinpoint the root cause at that time.
Tracing the Source
McKay began visiting other locales with similar staining issues in search of answers. In Oakley, Idaho, he learned that children’s teeth became brown after the town built a pipeline to a warm spring. When the pipeline was switched to a different spring, the staining vanished. In Bauxite, Arkansas, another community where stained enamel was common, McKay found a link to the town’s role as a center for aluminum production. This discovery connected the issue to the mineral bauxite, the source of aluminum. It was a moment when science became entangled with corporate interests.
"Whoever heard of fluorides in water? You have contaminated the sample. Rush another specimen." – Dr. H.V. Churchill
Dr. H.V. Churchill, ALCOA’s chief chemist, initially dismissed the idea of fluoride contamination but eventually found "surprising levels of fluoride" in the water. Testing water samples from Colorado Springs revealed similar results. [1] After nearly 30 years of work, McKay finally identified the cause of the blackened teeth: fluoride in the water, which caused a condition now known as fluorosis.
Understanding Fluorosis
The discovery of fluoride as the culprit spurred more questions. How could a substance that discolored teeth also make them more decay-resistant? How much fluoride was safe? Dr. H. Trendley Dean, head of dental research at the National Institute of Health, led pivotal studies to determine fluoride’s effects. He warned that individual susceptibility varied:
“The same amount of fluorine that causes a mild toxic reaction in one individual may cause a severe reaction in another.”
He suspected that if fluoride levels stayed below a certain threshold, you could enjoy cavity-preventing benefits without risking unsightly staining.
To test his hypothesis, Dr. Dean and his team studied four towns in Illinois. Two, Galesburg and Monmouth, shared a water source with 1.7 parts per million (ppm) fluoride and had far lower rates of dental caries (cavities) than Macomb and Quincy, which had only 0.02 ppm. Yet, when fluoride levels exceeded around 1 ppm, signs of fluorosis began to appear. The challenge was to strike a balance: too little fluoride didn’t protect against cavities, and too much risked the brown stains that had plagued Colorado Springs. The team concluded that fluorosis appeared when fluoride levels exceeded 1 ppm.
First Fluoridation Trial in Grand Rapids
Armed with these insights, Dr. Dean sought permission from Grand Rapids, Michigan, to add fluoride to its municipal water. Over 11 years, he monitored the children’s dental health. Results were remarkable: the caries rate dropped by over 60%, offering some of the most substantial evidence that fluoride could make dental caries a preventable disease. The Centers for Disease Control and Prevention later heralded water fluoridation as one of the 20th century’s major public health victories.
Before the mid-1940s, most Americans' only consistent source of fluoride was whatever trace existed naturally in their water. Four widely referenced studies comparing paired cities—where one city’s water was fluoridated and the other’s was not—bolstered the case. One example was the Newburgh-Kingston Caries Fluorine Study in New York, starting in 1944.
Newburgh-Kingston Caries Fluorine Study
In 1944, sodium fluoride was added to Newburgh’s water, bringing its fluoride level to 1 ppm. Kingston, 30 miles away with a similar population of 30,000, was left at its naturally low fluoride level. Approximately 3,400 children in Newburgh and 2,800 in Kingston (aged 6-12) served as the study population. After three years, the number of decayed, missing, or filled (DMF) teeth per 100 in Newburgh fell from 21 to 14.8—a substantial decline—while Kingston’s numbers stayed the same.
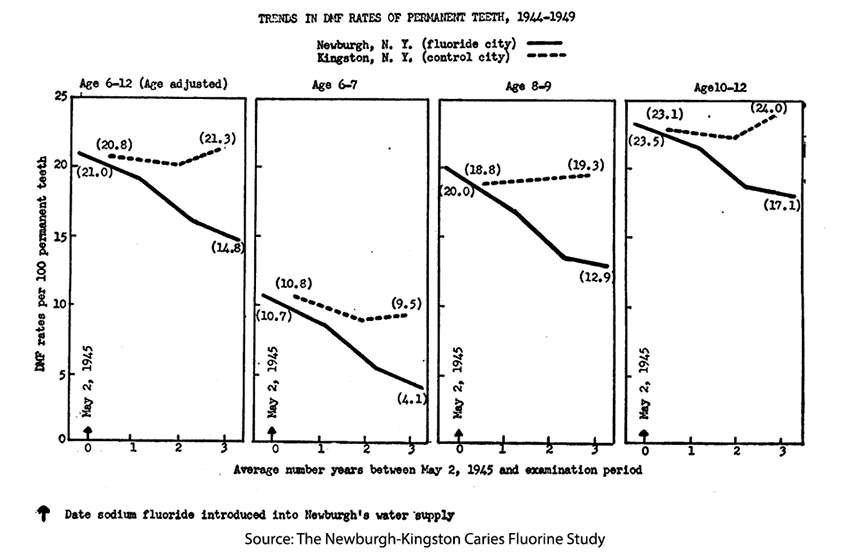
Further breakdown showed that the first permanent molars, typically most prone to decay, saw an 18% reduction in caries in Newburgh. The more resistant anterior and lateral incisors, which erupt soon after those first molars, fared even better, experiencing a 55% reduction. This correlation between water fluoride levels and cavity prevention reinforced earlier findings. It also raised a question that continues to befuddle: Is the effect of fluoride topical or systemic? – the protection of newly erupted teeth suggests that it is systemic.
Criticisms and Debates
Despite these promising results, water fluoridation faced criticism. Methodological concerns arose: Were the study designs rigorous enough? Congressman A.L. Miller of Nebraska, once an advocate of fluoridation, voiced worries about adults and individuals with kidney problems since fluoride is eliminated via urine.
Skepticism persists. In the 1980s, Nature highlighted a puzzling phenomenon in Western Europe, where fluoride was seldom added to water. Yet, rates of dental decay were falling to levels comparable to those in fluoridated countries. Moreover, for children “optimally exposed” since birth to about 1 ppm fluoride, caries continued to drop over time, suggesting that factors beyond water fluoridation—such as better oral hygiene, wider use of toothpaste, and more frequent dental checkups—could also be contributing.
An important historical context is that Americans adopted daily toothbrushing habits following World War II. Mass distribution of toothbrushes and toothpaste to military personnel introduced hygiene practices that often continued post-service. So, while fluoride played a key role, behavioral changes also transformed dental health outcomes.
Official Endorsement and Rapid Adoption
In 1950, Bruce Forsyth, Chief Dental Officer of the U.S. Public Health Service, told the American Dental Association that
"the fluoridation of public water supplies … can be encouraged subject to the approval of the State and local health authorities and the dental and medical profession." [emphasis added]
For a generation forged in war, when government leadership was essentially unquestioned, and teamwork was ingrained, simple encouragement was sufficient. No further marching orders needed to be given to care for your platoon or community. In 1950, approximately 1 million children were using fluoridated water; it grew three-fold by 1951, and by 1954 had reached 20 million children. Today, 77% of the population drinks fluoridated water.
A significant development occurred in 1956 with the introduction of Crest, the first toothpaste containing a fluoride additive. Perhaps you remember this television ad. Initially, Crest used stannous fluoride—branded “Fluoristan”—but later switched to sodium fluoride, known as “Fluoristat.” Because fluoride confers a clear therapeutic effect, the toothpaste was no longer merely a cosmetic product but was deemed a “drug delivery system,” requiring approval by the Food and Drug Administration (FDA). Procter & Gamble funded clinical trials with researchers from the University of Indiana’s Dental School.
Some 800 parents of children aged 6 to 15 in Bloomington, Indiana, were recruited, with 514 completing the six-month study. Half used stannous fluoride toothpaste, while the control group used fluoride-free. The stannous fluoride group showed a 53% reduction in decayed, missing, or filled teeth and a 72% reduction in decayed, missing, or filled tooth surfaces. The American Dental Association (ADA) granted its official seal of approval—Crest was the first toothpaste, but not the last, to be
"… shown to be an effective decay-preventive dentifrice that can be of significant value when used in a conscientiously applied program of oral hygiene and regular professional care.”
Public Perception and Trust in Government
By 1998, roughly 70% of people polled by the ADA believed community water should be fluoridated. However, lingering doubts remained. A survey of approximately 5,000 participants explored perceptions of fluoride’s safety and benefits. It found that:
- 55% agreed or strongly agreed that fluoridated water was safe; 31% were neutral; 13% disagreed or strongly disagreed.
- 57% believed there was some health benefit, 15% believed the benefit was significant, and 27% saw no benefit.
- 50% were unsure of fluoride’s role in dental health.
- The highest agreement on the safety of community water fluoridation was among those who knew of fluoride's role (96%), and the greatest disagreement was among those who felt that childhood vaccines were unsafe (65%).
The study noted a connection between negative views on community water fluoridation (CWF) and distrust of vaccines. People who believed vaccines were unsafe were likelier to reject fluoridation. In other words, trust in government-endorsed health measures proved a critical determinant of public acceptance. That distrust was first noted in this classic depiction from the movie Dr. Strangelove.
These insights echo many modern debates around public health, in which individual autonomy, suspicion of government authority, and variable acceptance of scientific evidence collide. Supporters point to fluoridation’s decades-long track record in reducing dental caries across populations, while critics worry about potential side effects, overreach by government, and the possibility that some subpopulations could be more vulnerable to chronic fluoride exposure.
Legacy and Ongoing Questions
While fluoridation’s effect on reducing cavities is no longer seriously in doubt, the precise contribution of water fluoride compared to better brushing habits, fluoride toothpaste, professional dental care, and improvements in diet remain a subject of study. These myriad factors likely act in concert—one reason developed nations have seen a broad decline in tooth decay, regardless of whether they fluoridate.
Nevertheless, few public health interventions have achieved the same impact as water fluoridation. From the vantage point of modern dentistry, the story’s arc—from those early days in Colorado Springs through Bauxite, Arkansas, to the introduction of fluoride toothpaste—shows how scientific curiosity, persistent investigation, and public policy can work together to improve health on a massive scale.
Despite controversies and debates about dosage, safety, and personal freedom, the conclusion drawn by many health organizations remains. When properly regulated, fluoride in water and toothpaste remains a highly effective, low-cost way to prevent tooth decay for entire communities.
[1] Colorado Springs is an area that contains the mineral cryolite, which in turn contains fluoride. Runoff from rain and snow dissolved the fluoride, contaminating the drinking water.
Sources: The Story of Fluoridation



